BAD HOFGASTEIN, Austria — Belgium, which takes over the presidency of the Council of the European Union in January 2024, plans to make the healthcare workforce crisis a central item on its agenda, the first time the issue will be prioritized at the highest level of EU policymaking in over a decade.
“We are actively considering the health workforce and all the challenges around health workforces to be one of the main priorities of the Belgian presidency,” Lieven De Raedt, a strategic advisor on the international unit of the Belgian Federal Ministry of Health, told the European Health Forum in Gastein, Austria, on Thursday.
De Raedt stressed that the Belgian presidency’s agenda is not yet finalized, but confirmed to Health Policy Watch that Belgium will push for an ambitious approach to the future direction of EU health policy.
The Belgian presidency will aim to make the health workforce crisis “one of the main priorities at the EU level for the upcoming years and the next Commission”, De Raedt told the conference.
Internal dialogues held by Belgian delegations with EU health ministers to determine the priorities of the country’s presidency of the Council of the European Union found that the health workforce crisis is the “main headache for basically all health ministers in the EU and in the WHO European region,” De Raedt said.
“It is obvious that this is the main challenge in health policy,” he added.
The clock is ticking on Europe’s health workforce crisis

A rapidly ageing population is putting increasing pressure on European health systems, as the bloc struggles to retain its current health workforce. Alarming numbers of health workers are fleeing to other sectors due to poor working conditions, low pay, and threats to their physical and mental health exacerbated by the strains of the COVID-19 pandemic.
The World Health Organization (WHO) has warned that Europe’s health workforce crisis is a “ticking time bomb”.
Countries in the WHO’s European region, which stretches from the United Kingdom to the plains of Kyrgyzstan and Tajikistan in Central Asia, currently face a shortfall of 1.8 million health workers, and that number is expected to double to 4 million by 2030.
“The number one problem is the health worker crisis we have here in Europe because there is no health without the health workforce,” Dr Hans Kluge, WHO regional director for Europe said on Wednesday.
Young doctors on the frontlines of the crisis say the numbers bear out a stark reality on the ground facing healthcare workers who want to stay in the health workforce.
“The most important part for us is to retain our workforce,” Alvaro Cerame, chairperson for the Medical Workforce Committee of the European Junior Doctors Association (EJD), told Health Policy Watch. “Our generation does not only have to take care of our children, but because of the demographic changes, we also have to take care of our elders – and with fewer social support structures.”
A meeting of EU health ministers in 2010 saw the crisis coming

Thirteen years after a meeting of European Union health ministers warned of an impending crisis in the bloc’s health workforce, the situation has worsened as EU governments failed to act on the warning signs.
The outcome document of a 2010 ministerial meeting – titled “Investing in Europe’s health workforce of tomorrow” – called on the bloc’s member states to “invest in sufficient, motivated and well-skilled health professionals in order to protect the viability and accessibility of health systems.”
EU health ministers have not convened to discuss the health workforce crisis since 2010, when Belgium last held the presidency of the EU Council.
While the EU has held consultations and launched projects on health worker migration, skills, empowerment, and workforce planning and forecasting in the years since that meeting, the bloc’s health workforce remains chronically underfunded.
The EU’s 2021 health budget, EU4Health, was the largest ever allocated to the sector, at €5.3 billion. But over half, €2.8 billion, is earmarked for DG HERA, the European Commission’s health emergency preparedness and response unit created to combat COVID-19. Most of this money has been spent on medical countermeasures against the virus such as vaccines.
A modest €2.5 billion is left for non-crisis health spending, with almost none of it going to the health workforce.
“The EU4Health program is €5.3 billion, and so far, only about €10 million has been spent on the health workforce, which is somewhere between 0.1% and 0.2%,” said De Raedt. He emphasized that his calculations are preliminary and do not reflect the official stance of the Belgian government.

EU underinvestment in health workforces stems from their long-held status as a national-level issue, rather than one for EU decision-makers in Brussels. This has left EU countries without a coordinated response to the health workforce crisis.
“Anytime we try to discuss this, at least from my experience, it always devolves into ‘this is a national competence’,” Sara Cerdas, a Portuguese medical doctor and MEP for the European Socialist party, told Health Policy Watch.
“Whereas, as I see it, we should have an EU approach on this because we cannot see 27 health systems in silos and then protect public health together.”
This has exacerbated the crisis in less developed EU countries, such as Bulgaria, which produces many doctors and nurses but loses them to richer countries within the bloc whose health systems can offer higher salaries.
“It is a no-brainer that the health workforce is a public good across EU member states,” Josep Figueras, director of the European Health Observatory told Health Policy Watch. “If professionals can cross borders, we need to work together [because] unfortunately the migration is only going in one direction.”
Threats identified a decade ago fuelling today’s health workforce crisis

The 2010 ministerial meeting in La Hulpe, a leafy suburb on the outskirts of Brussels, predicted the outlines of Europe’s current health workforce crisis with astounding precision.
The outcome document warned of the urgent need to improve “forecasting future health workforce needs” through the collection of “high-quality and comparable data” across the EU.
Today, this remains one of the bloc’s biggest blind spots, according to Sandra Gallina, Director General for Health and Food Safety at the European Commission.
“I am a numbers person, and I can tell you we need to improve the measuring of where we are, what we need and where we should be going,” Gallina said at a closed-door media briefing on Wednesday.
“We need to be better at planning and forecasting needs for the workforce – there are medical deserts already appearing,” she added, referring to geographic areas across the EU where people have limited or no access to healthcare services due to staffing shortages.
Another problem identified by the ministerial meeting – “the ageing of the population and of the health workforce” – has not gone away, either.
Europe’s medical workforce is ageing at a staggering rate. Across Europe, the average doctor is over 55 years old. In 13 countries, at least 40% of doctors are over 55 and will retire within the next decade. Italy has the oldest medical workforce in Europe, with nearly 60% of doctors over 55.
“That means that in the next few years, more than 40% of these doctors will be retiring,” Tomas Zapata, unit lead for health workforce and health services at WHO’s European Office said on Thursday.
“That’s a tsunami of retirements,” said Zapata.
Doctors under mounting pressure
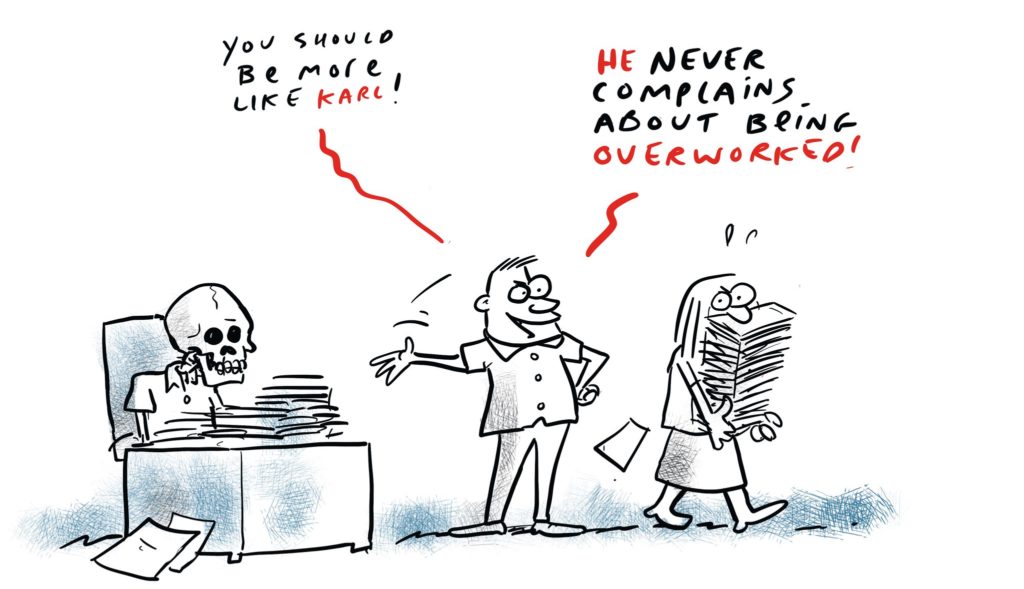
As Europe’s doctors retire and burn out at a rapid pace, the remaining workforce is coming under increasing pressure.
Alvaro Cerame, the young Spanish doctor chairing the European Junior Doctors Association’s Medical Workforce Committee, said it is not uncommon for doctors who come in for 24-hour on-call shifts to continue working without a break up to 36 hours.
The 2010 meeting identified this problem as well, stressing the “importance of attractive working environments [and] working conditions” for “guaranteeing the quality and safety of the care provided”.
This overstretched workforce is not only harming doctors, nurses, and other healthcare workers but also actively endangering patients.
“There is no doubt that when you work for so many hours — like in any sector — you will not be able to provide quality care, and it is going to put patients at risk,” Cerame said. “States and healthcare systems need to provide safe working conditions for healthcare workers and safe conditions for the patients who are in the healthcare system.”
Where are nurses and medical graduates going?

The paradox of Europe’s health worker crisis is that there are more doctors, nurses, and other health workers than ever working in health systems across the region.
The WHO European region has the most doctors and nurses per capita in the world. Over the past eight years, the region has seen an 8% increase in the density of doctors and a 12% increase in the density of nurses per capita.
But these impressive gains mask a hidden problem: nursing and medical school graduates are not staying in the workforce.
Despite a 37% increase in medical graduates and a 26% increase in nursing graduates in the WHO European region over the past decade, the number of healthcare workers has not kept pace with demand. In fact, Europe’s medical and nursing graduate output has outpaced workforce growth by 29% and 14%, respectively.
The gap is even wider than the WHO figures suggest, as Europe also imports a significant number of healthcare workers from lower-income countries in Africa and Asia. These workers face even bigger retention challenges due to migration policies and visa requirements.
So where are Europe’s medical and nursing graduates going?
“Nobody knows. We have around 30% [of graduates] that are missing somehow, people who are trained but not retained in the health care workforce,” Francisco Ribeiro Mourão, treasurer of the European Junior Doctors Association (EJD), told Health Policy Watch.
The EJD has been trying to fill this knowledge gap and will release a report on the European healthcare workforce next month. But for now, it remains unclear which sectors are gaining the nursing and medical graduates that the health workforce is losing.
“In Austria, for example, like 30% of medical students don’t enter the workforce,” Antatas Montvila, vice president of the EJD and a radiologist in Lithuania, told Health Policy Watch about the findings of the report.
The European Health Observatory’s Figueras cautioned that the report’s methodology and findings, which are not yet public, may require further analysis, telling Health Policy Watch that burnout and workforce migration are the likeliest causes for the gap identified in the report.
Whatever the cause, Europe’s front line doctors see a system that is failing them and their patients.
“According to our research and communicating with our members, we feel that these recent resignations were more or less like silent protests,” Montvila said. “The health system is failing, and it is extremely inefficient.”
“The previous generation, they will still tend to work overtime or in their free time,” Montvila concluded. “But I think that juniors are starting to understand that they are not personally responsible for a failing system.”
‘It’s democracy, man’
European Commission officials, health experts, and politicians say that the bloc has the tools to fix its health workforce crisis, but pressure from civil society and voters across Europe must increase if the issue is to rise to the top of the agenda.
“Member states need to ask the Commission, need to ask the elected politicians to push this agenda because the tools are there – it’s all there, it’s just political will, bloody political will,” said Figueras.
“We need civil society, we need the press, we need a bottom-up push from member states for the EU to take [it] on,” Figueras added.
Sara Cerdas, the Portuguese doctor and MEP, agreed that pressure from civil society is key, noting the dominance of direct messaging to EU politicians from lobbyists and interest groups compared to its citizens.
“There needs to be more pressure to discuss this at the EU level, and we cannot do that alone as politicians,” said Cerdas.
Gallina, one of the EU’s most senior health officials, echoed a similar sentiment on Wednesday, saying the EU is ready to take action.
“We are all watching this space,” said Gallina. “This is also a matter for voters and citizens to take into their hands.”
“It’s democracy, man,” Gallina said.
Source: Health Policy